Muscle relaxants, along with volatiles, induction agents, local anaesthetics and opiates, are some of the drugs which require the greatest depth of knowledge for the Primary FRCA. Muscle relaxants are classified into two overarching groups; depolarising muscle relaxants and non-depolarising muscle relaxants.
Here on TeachMeAnaesthetics, we aim to cover the absolute key details of high yield exam topics, which can then be supplemented with further reading as needed.
In this article, we will discuss the classification, mechanisms and key features of the non-depolarising muscle relaxants used in UK anaesthetic practice.
The Ideal Muscle Relaxant
“Tell me, what are the properties of the ideal induction agent/muscle relaxant/opiate/volatile agent?” asks the examiner, in what is (anecdotally) a bread-and-butter start to a viva question. In this case, your answer might feature some of the following points:
Physical properties
- Stable with a long shelf life
- Can be stored at room temperature
- Readily available
- Painless on injection
- Predictable onset and offset times
- Reversible
- Minimal interaction with other agents
Biological properties
- Free of unwanted side effects
- Non-toxic
- Analgesic
Classification of Non-Depolarising Muscle Relaxants
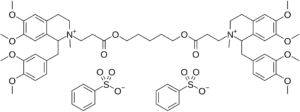
The non-depolarising agents can be further categorised according to their chemical structure, into the aminosteroids and the benzylisoquinoliniums. As can be inferred from their name, the aminosteroids consist of an amine-substituted steroid nucleus, while the benzylisoquinoliniums are based upon benzylisoquinoline (you would not be expected to draw these!).
Importantly, the different structures confer different pharmacokinetic and pharmacodynamic profiles; which we will now explore further.
Aminosteroids
The aminosteroids include rocuronium, pancuronium and vecuronium. Compared to the benzylisoquinoliniums, they cause less histamine release. Their steroid ring structure also serves as a target for sugammadex, so they are more rapidly reversible.
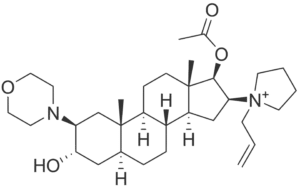
Figure 1
Rocuronium, with its amine substituted steroid ring
Benzylisoquinoliniums
The benzylisoquinoliniums include atracurium, cis-atracurium (a specific stereoisomer of cisatracurium), and mivacurium. As stated, they cause more histamine release than their aminosteroid counterparts, and so should be used with caution in those with poorly controlled asthma or COPD.
Pharmacokinetics
In brief, muscle relaxants are bulky and charged molecules. This significantly limits their diffusion across biological membranes. As a result, they do not cross the blood-brain barrier and do not cross the placenta in clinically significant amounts.
Pharmacodynamics
Mechanism of Action
In order to appreciate how non-depolarising agents work, a brief dive into the physiology of the neuromuscular junction is necessary.
Upon the arrival of an action potential at the pre-synaptic membrane, acetylcholine is released into the synapse. This diffuses across the synapse to meet a nicotinic acetylcholine receptor on the post-synaptic membrane.
The adult nicotinic acetylcholine receptor is a pentameric structure, consisting of two alpha, one beta, one epsilon and one delta subunit (the epsilon subunit replaces the gamma subunit that was present in the foetus). Following the binding of two acetylcholine molecules to the alpha subunits, a conformational change occurs, which opens up a central pore. Through here, sodium ions are able to flow, which depolarises the post-synaptic neurone and facilitates the conduction of an action potential.
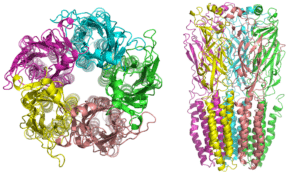
Figure 2
Diagram of the nicotinic receptor, showing the 5 subunits and the central pore
Non-depolarising agents act as competitive antagonists by binding to the alpha subunit and inhibiting the binding of acetylcholine. Therefore, the propagation of the action potential across the neuromuscular junction is inhibited, and muscles are no longer able to contract.
Clinical Relevance
Potency and Speed of Onset
Out of the non-depolarising agents, why is only rocuronium suitable for an RSI? The answer to this question lies in its potency.
By way of recap, potency describes the dose of an agent required for a given clinical effect. A highly potent agent requires a lower dose than a less potent agent for the same effect to be achieved.
Rocuronium has the lowest potency of the non-depolarising muscle relaxants, and therefore must be given in a higher dose. As a result, a greater concentration gradient is achieved between the plasma and the neuromuscular junction.
A greater concentration gradient leads to a more rapid rate of diffusion, and thus a more rapid onset which facilitates a speedier intubation.
Specific Muscle Relaxants – Aminosteroids
Rocuronium
- Dose of 0.6mg/kg for normal induction, 1.2mg/kg for RSI.
- Duration ~45 mins
- Excreted in bile (60%) and urine (40%). Duration of action may increase in hepatic and renal failure.
- Reversible by sugammadex
Vecuronium
- Dose of 0.1mg/kg.
- Duration ~45 mins
- Excreted in bile (70%) and urine (30%)
- Reversible by sugammadex
Pancuronium
- Bisquaternary structure, more charged than rocuronium and vecuronium
- Dose of 0.1mg/kg
- Long duration of action (~100 mins)
- 80% eliminated in urine, 20% in bile
- Technically reversible by sugammadex but no dose given on product sheet
Specific Muscle Relaxants – Benzylisoquinoliniums
Atracurium
- Dose of 0.5mg/kg
- Metabolised by ester hydrolysis (60%) and Hofmann degradation (40%)
- Hofmann degradation is slowed by hypothermia and acidosis
- Causes histamine release
- Duration of action roughly 20-30 minutes
Cis-atracurium
- One of 10 stereoisomers of atracurium
- More potent, with a dose of 0.2mg/kg
- Less histamine release
- Duration of action roughly 20-30 minutes
Mivacurium
- Dose of 0.2mg/kg
- Short acting (15-20 minutes)
- Metabolised by ester hydrolysis through plasma cholinesterases – may be prolonged in those with suxamethonium apnoea
- Use is declining as can be unpredictable in its onset and offset
Suggested Reading
Chapter 19. Primary FRCA Structured Oral Examination Study Guide 2. Second edition. McCombe and Wijayasiri. 2016.
Chapters 4.15-4.16. Graphic Anaesthesia. 2nd Edition. Hooper, Nickells et al. 2023.
E-LFH session: https://portal.e-lfh.org.uk/Component/Details/692562