There are few more fundamental pieces of equipment in modern anaesthetic practice than the humble pulse oximeter. In recognition of its importance, a detailed understanding of pulse oximetry is expected for the Primary FRCA examinations.
Here on TeachMeAnaesthetics, we aim to cover the absolute key details of high yield exam topics, which can then be supplemented with further reading as needed.
In this article, we will cover how pulse oximetry works, with a discussion of the underlying physical principles.
Pulse Oximetry
Pulse oximetry describes the non-invasive measurement of oxygen saturations using photoplethysmography. While this long word may appear intimidating, it helpfully describes the underlying principles of pulse oximetry:
- Photo-: Light of different wavelengths is used to elicit the oxygen saturations of haemoglobin
- -plethys: Refers to the measurement of a change in volume i.e. the arterial pulse is detected
- -mography: A waveform is generated, which has its own utility. The position of the dicrotic notch can be a surrogate measure of afterload, and the degree of ‘swing’ on the SpO2 trace can be indicative of hypovolaemia.
The Beer-Lambert Law
The Beer-Lambert law is a composite of two separate laws.
- Beer’s law states that the absorbance of radiation as it passes through a substance is proportional to the concentration of said substance.
- Lambert’s law states that the absorbance of radiation as it passes through a substance is proportional to the distance travelled through said substance. (Think Lambert = length and the two sort themselves out in terms of which is which)
Together, the Beer-Lambert law therefore describes how with an increasing concentration of a substance, and a longer path through which light must travel, a greater degree of light will be absorbed and therefore less will be detected at a distal photodetector.
How Pulse Oximetry Works
LEDs
A pulse oximeter consists of two sets of light emitting diodes (LEDs), which emit light at frequencies of either 660 nm or 940 nm (red and infrared light respectively) into the target tissue. These flicker on and off rapidly, and the degree of absorbance of each respective wavelength is measured at a photodetector on the opposite side of the finger/ear.
The sequence at which the LEDs are active is important. They rotate through a sequence of on/off, off/on, off/off thirty times a second. During the off/off stage, the pulse oximeter knows that there is no deliberately emitted light; this allows for the effect of any ambient light to be accounted for.
Wavelengths
Why are those two remarkably specific wavelengths of 660 and 940 nm used? The answer lies in the absorption spectra of oxyhaemoglobin and deoxyhaemoglobin.
At 940 nm, which lies on the infrared portion of the light spectrum, oxyhaemoglobin absorbs light to a much greater degree than deoxyhaemoglobin. The converse is true at 660 nm; deoxyhaemoglobin preferentially absorbs light here to a much greater degree than oxyhaemoglobin.
By using points at which the behaviour of oxyhaemoglobin and deoxyhaemoglobin differ significantly, a more reliable estimate of oxygen saturations can be generated.
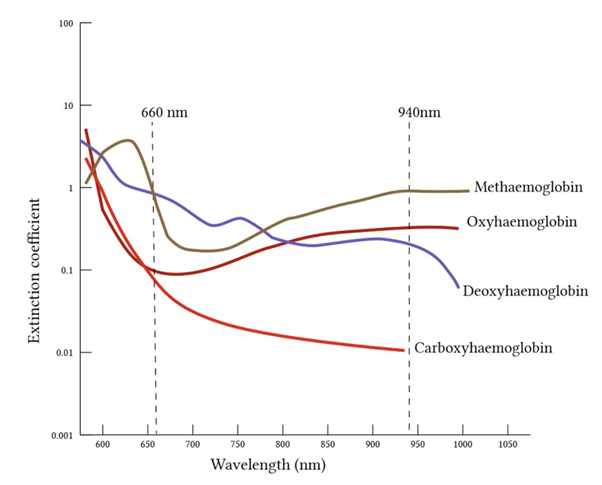
Figure 1
Absorbance according to wavelength and haemoglobin subtype
Isobestic Point
Simply put, the isobestic point is the point at which the absorbance of light is the same for both oxy- and deoxyhaemoglobin. There are two isobestic points – one at 590 nm, and one at 805 nm.
There isn’t much more to be said about them, but an awareness of their existence is expected in the Primary FRCA.
Determining Oxygen Saturations
Once the photodetector has figured out the relative absorbance of both oxy- and deoxyhaemoglobin, a ratio of the two is generated. An algorithm is then used to derive the oxygen saturations.
As an aside, when the pulse oximeter was being developed, it was calibrated by deliberately inducing hypoxia in healthy volunteers. For obvious reasons, there is a lower limit to which this can be done safely, and therefore the ‘lowest’ accurate SpO2 is ~70%. Below that, it’s guesswork.
Determining the Pulse
As a pulse of blood is delivered to the finger, both the concentration of oxyhaemoglobin and the thickness (i.e. the pathway length) of the finger increase.
Using the Beer-Lambert law, we can expect the absorbance of light to increase as a result.
By comparing the relative absorbances during systole and diastole, the pulse rate can be calculated. As above, the waveform generated can also be used to provide surrogate measures of afterload and hypovolaemia through the dicrotic notch and the degree of ‘swing’ respectively.
Advantages and Disadvantages of Pulse Oximetry
Advantages
- Easy to use
- Safe
- Non-invasive
- Continuous measurement
Disadvantages
- Unreliable below 70% oxygen saturations
- Unreliable in arrhythmias
- False measurements in the presence of carboxyhaemglobin (falsely high) and methaemoglobin (falsely fixed around 85%)
- Can cause pressure sores and burns
- Can be unreliable in those with darker skin
Suggested Reading
Chapter 6.10. Equipment in Anaesthesia and Critical Care: A complete guide for the FRCA. Aston, Rivers, Dharmadasa. 2014.
Chapter 82. The Primary FRCA structured oral examination Study Guide 1. 2nd edition. Wijayasiri and McCombe. 2016.
BJA article: https://www.bjanaesthesia.org/article/S0007-0912(22)00134-9/fulltext